What is Respiratory Compromise?
The concept of respiratory compromise is not new the respiratory therapy or to health care. However, there is a need for ongoing research so that the exact scope, range of etiologies, incidence and severity can be better understood. 2
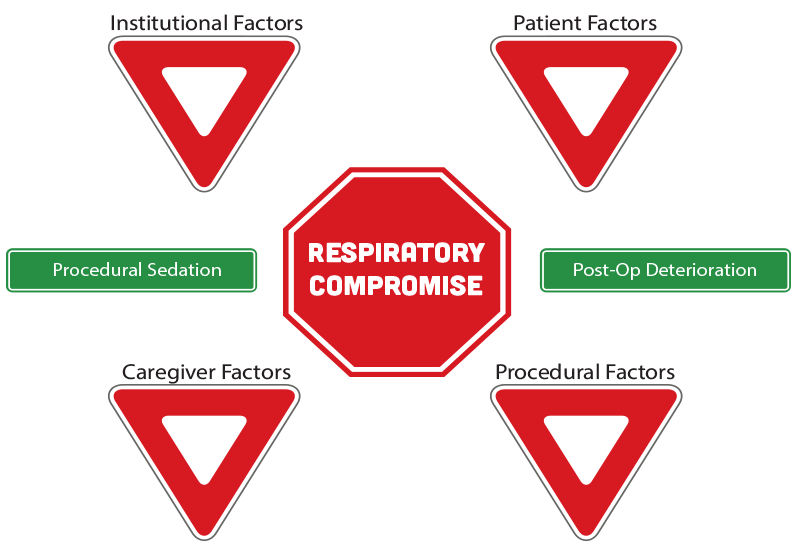
There exists a growing body of literature on respiratory compromise in certain patient care contexts. The CSRT has opted to focus on two priority areas based on the evidence in the literature: procedural sedation and post-operative respiratory deterioration.
1Morris, TA, Gay, PC, MacIntyre, NR., Hess, DR, Hanneman, SK, Lamberti, JP, Doherty, DE, Chang, L, and Seckel, MA. (2017). Respiratory compromise as a new paradigm for the care of vulnerable hospitalized patients. Respir Care 62 (4) 497-512; DOI: https://doi.org/10.4187/respcare.05021 http://rc.rcjournal.com/content/62/4/497.short
2Correia, R, Wnuk, A., Zaccagnini, M., West, A. (2019). Actioning our understanding of respiratory compromise Can J Respir Ther 55:28-29. https://www.cjrt.ca/wp-content/uploads/doi-10.29390cjrt-2018-026.pdf
Click on the various shapes for more information.
Institutional Factors
Institutional risk factors for respiratory compromise include underfunding, a distant location of monitoring stations or equipment relative to staff and patients, various environmental factors (noise, lighting, temperature) and a lack of protocols relating to medication administration and patient monitoring.
References
Association for the Advancement of Medical Instrumentation. (2010). Infusing patients safely: priority issues from the AAHI/FDA infusion device summit. Arlington: AAMI.
Canadian Medical Protective Association. (2016, September). Safe use of opioid analgesics in the hospital setting. Retrieved from Canadian Medical Protective Association: https://www.cmpa-acpm.ca/en/advice-publications/browse-articles/2016/safe-use-of-opioid-analgesics-in-the-hospital-setting
Lynn, L. A., & Curry , J. P. (2011). Patterns of unexpected in-hospital deaths: a root cause analysis. Patient Safety in Surgery, 5(3).
Patient Factors
Patient-related factors that elevate the risk of respiratory compromise include the patient’s age (with the very young and the elderly at highest risk), history of cigarette/alcohol use and the need for medications that suppress the drive to breathe (e.g. opioids). Patients who require airway protection or intubation and those who do not understand their course of treatment (procedures, medications, risks, etc.) are also at elevated risk for respiratory compromise. The following comorbidities are also associated with an increased risk: cardiovascular, lung, liver, kidney or neuromuscular disease; cancer, diabetes, obesity, sepsis, organ dysfunction/failure; CNS injury or disease; chest cage dysfunction; sleep disordered breathing.
References
Alvarez, M. P., Samayoa-Mendez, A. X., Naglak, M. C., Yuschak, J. V., & Murayama , K. M. (2015). Risk factors for postoperative unplanned intubation: analysis of a national database. The American Surgeon, 81(8), 820-825.
Morris, T. A., Gay, P. C., MacIntyre, N. R., Hess, D. R., Hanneman, S. K., Lamberti, J. P., . . . Seckel, M. A. (2017). Respiratory compromise as a new paradigm for the care of vulnerable hospitalized patients. Respiratory Care, 62(4), 497-512.
Ramchandran, S. K., Nafiu, O. O., Tremper, K. K., Shanks, A., & Kheterpal, S. (2011). Independent predictors and outcomes of unanticipated ealry postoperative tracheal intubation after nonemergent, noncardiac surgery. Anesthesiology, 115(1), 44-53.
Weingarten, T. N., Herasevich, V., McGlinch, M. C., Beatty, N. C., Christensen, E. D., Hannifan , S. K., et al. (2015). Predictors of delayed postoperative respiratory depression assessed from naloxone administration. Anesthesia and Analgesia, 121(2).
Caregiver Factors
Caregiver risk factors for respiratory compromise include communication barriers within the healthcare team, alarm fatigue, improper/insufficient education or training, medication errors and caregiver fatigue/illness.
References
Association for the Advancement of Medical Instrumentation. (2010). Infusing patients safely: priority issues from the AAHI/FDA infusion device summit. Arlington: AAMI.
Canadian Medical Protective Association. (2016, September). Safe use of opioid analgesics in the hospital setting. Retrieved from Canadian Medical Protective Association: https://www.cmpa-acpm.ca/en/advice-publications/browse-articles/2016/safe-use-of-opioid-analgesics-in-the-hospital-setting
Lynn, L. A., & Curry , J. P. (2011). Patterns of unexpected in-hospital deaths: a root cause analysis. Patient Safety in Surgery, 5(3).
Procedural Factors
Patients who have recently undergone a long or complicated procedure requiring anesthesia, sedation or pain-relieving medications or patients who required a blood transfusion during surgery are at increased risk of respiratory compromise.
References:
Alvarez, M. P., Samayoa-Mendez, A. X., Naglak, M. C., Yuschak, J. V., & Murayama , K. M. (2015). Risk factors for postoperative unplanned intubation: analysis of a national database. The American Surgeon, 81(8), 820-825.
Weingarten, T. N., Herasevich, V., McGlinch, M. C., Beatty, N. C., Christensen, E. D., Hannifan , S. K., et al. (2015). Predictors of delayed postoperative respiratory depression assessed from naloxone administration. Anesthesia and Analgesia, 121(2).
Respiratory Compromise
Evidence
(Note: Some links are to abstracts only.)
Morris, TA, Gay, PC, MacIntyre, NR., Hess, DR, Hanneman, SK, Lamberti, JP, Doherty, DE, Chang, L, and Seckel, MA. (2017). Respiratory compromise as a new paradigm for the care of vulnerable hospitalized patients. Respir Care 62 (4) 497-512; DOI: https://doi.org/10.4187/respcare.05021
http://rc.rcjournal.com/content/62/4/497.short
Correia, R, Wnuk, A., Zaccagnini, M., West, A. (2019). Actioning our understanding of respiratory compromise Can J Respir Ther 55:28-29. https://www.cjrt.ca/wp-content/uploads/doi-10.29390cjrt-2018-026.pdf
Clinical Resources
Risk Factors for Respiratory Compromise printable:
Click Here to Download this PDF FIle
Moskowitz A, Andersen LW, Karlsson M, et al. Predicting in-hospital mortality for initial survivors of acute respiratory compromise (ARC) events: Development and validation of the ARC Score. Resuscitation 2017;115:5–10. doi: 10.1016/j.resuscitation.2017.02.022.
Click Here to Download this PDF FIle
Educational Resources
CSRT Webinar: Respiratory Compromise: Common, Costly, Deadly and Preventable (Presented by Michael Mestek, Medtronic, October 11, 2017.) https://csrt.member365.com/sharingnetwork/education/video/13/1
CSRT Webinar: Monitoring for Respiratory Compromise (Presented by Cheryl St. Croix, Andrea Wnuk, Marco Zaccagnini, Carolyn McCoy November 9, 2017.) https://csrt.member365.com/sharingnetwork/education/video/16/1
Correia, R, Wnuk, A., Zaccagnini, M., West, A. (2019). Actioning our understanding of respiratory compromise Can J Respir Ther 55:28-29. https://www.cjrt.ca/wp-content/uploads/doi-10.29390cjrt-2018-026.pdf
Healthstream Capnography Structured Education Curriculum Video Series: (Free registration may be required to view these videos.): Click here to watch.
Capnography Waveforms (Interactive PDF) https://www.medtronic.com/covidien/en-us/clinical-education/catalog/interactive-pdf-capnography-waveforms.html
Priority area 1:Procedural Sedation
Evidence
(Note: Some links are to abstracts only.)Saunders R, Struys MMRF, Pollock RF, et al. Patient safety during procedural sedation using capnography monitoring: a systematic review and meta-analysis. BMJ Open 2017;7:e013402. doi:10.1136/ bmjopen-2016-013402 https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC5734204/pdf/bmjopen-2016-013402.pdf
Gallagher, JJ., Capnography monitoring during procedural sedation and analgesia. AACN Adv Crit Care. 2018 Winter;29(4):405-414. doi: 10.4037/aacnacc2018684. https://www.ncbi.nlm.nih.gov/pubmed/30523011
Clinical Resources
Recommendations of Clinical societies and Organizations: Standards and guidelines for capnography monitoring during procedural sedation https://www.csrt.com/wp-content/uploads/capnography-standards-guidelines-procedural-sedation-society-list.pdf
Dobson, G., Chong, M.A., Chow, L. et al. Procedural sedation: a position paper of the Canadian Anesthesiologists’ Society. Can J Anesth/J Can Anesth (2018) 65: 1372. https://doi.org/10.1007/s12630-018-1230-z
https://link.springer.com/article/10.1007/s12630-018-1230-z
Educational Resources
CSRT Webinar: Procedural Sedation and Capnography in the Specialty Suites (Presented by Erin McLaughlin, RRT [Medtronic], October 25, 2016.) https://csrt.member365.com/sharingnetwork/education/video/19/1
CSRT Webinar: L'EtCO2 en sédation procédurale - un outil facile et sécuritaire (Présenté par: Annie Bélanger, inh. [Medtronic] le 27 octobre 2016.) https://csrt.member365.com/sharingnetwork/education/video/23/1
Priority area 2: Post-Operative Deterioration
Evidence
(Note: Some links are to abstracts only.)Lam, T., Nagappa, M., Wong, J., Singh, M., Wong, D. Chung, F. (2017). Continuous pulse oximetry and capnography monitoring for postoperative respiratory depression and adverse events: a systematic review and meta-analysis. Anesthesia & Analgesia. 125 (6): 2019-2029. doi: 10.1213/ANE.0000000000002557 https://journals.lww.com/anesthesia-analgesia/fulltext/2017/12000/Continuous_Pulse_Oximetry_and_Capnography.31.aspx
Khanna A, Overdyk F, Greening C, Di Stefano P, Buhre W. Respiratory depression in low acuity hospital settings – Seeking answers from the PRODIGY trial. J Crit Care 2018;47:80–7. doi: 10.1016/j.jcrc.2018. 06.014. https://www.sciencedirect.com/science/article/abs/pii/S088394411830217X?via%3Dihub
Clinical Resources
Canadian Patient Safety Institute Enhanced Recovery after Surgery (ERAS) toolkit: https://www.patientsafetyinstitute.ca/en/toolsResources/Enhanced-Recovery-after-Surgery/Pages/default.aspx
Educational Resources
Anesthesia Patient Safety Foundation (2011). Monitoring for Opioid-Induced Ventilatory Impairment (video): https://www.apsf.org/videos/monitoring-for-opioid-induced-ventilatory-impairment-oivi-video/


